A diagnosis of dementia can be devastating, but the damage of an incorrect diagnosis has its own fallout. But how common is it to receive either a false diagnosis of dementia or a misdiagnosis for a specific type of dementia? As those who have dealt with dementia, there are several different types, each with its own set of treatment protocols and expected disease progression.
A recent study conducted by Australian researchers looked specifically at the frequency of misdiagnosis of frontotemporal dementia (FTD), comparing the initial referral data to the final clinical diagnosis, according to SciTechDaily.
The study reviewed the records of 100 patients referred to a memory disorders clinic by specialists. Researchers found that 70 percent of patients initially suspected of having frontotemporal dementia (FTD) were ultimately misdiagnosed.
Insights from the study:
- 34 patients were accurately diagnosed while 66 were false positive.
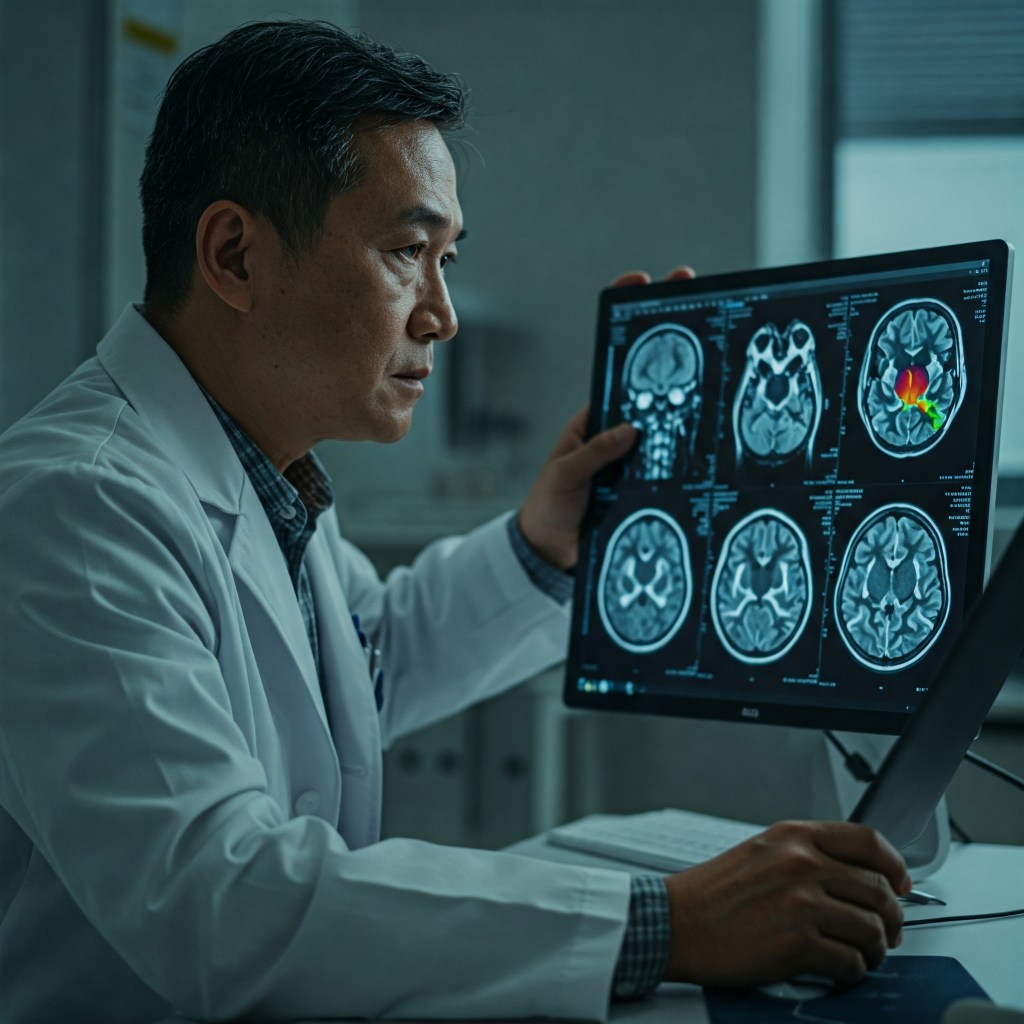
- Researchers determined that misinterpretation of neuroimaging, specifically nuclear imaging, was the primary cause of misdiagnosis of FTD.
- Cognitive testing also played a factor in misdiagnosis.
- Patients who presented with prior psychiatric histories were more likely to be misdiagnosed with FTD.
The study was small and based upon cases at a single clinic, so it’s difficult to know how widespread the issue of misdiagnosing FTD is in other countries.
FTD has been in the news this past week due to the ongoing saga of media personality Wendy Williams, who is claiming she doesn’t have FTD after reportedly being diagnosed and assigned a court-appointed guardian. There has been an ongoing controversy about the continued need for the legal conservatorship, and Williams is speaking out, frustrated by the lack of control she now has over her finances and living arrangements. As the above study found in some of the cases it reviewed, it may be possible that Williams was misdiagnosed with FTD and instead experienced alcohol-induced dementia, related to her well-documented struggles with alcohol, or another form of mental illness which had gone untreated. I am not a medical professional, but it seems reasonable that a second opinion and additional testing should be conducted, if it hasn’t already been done. If a celebrity like Wendy Williams can find herself in such a challenging situation, think about regular people like the rest of us who don’t have such a public platform to ask for help.
Image created by Google Gemini.



![Pageflex Persona [document: PRS0000038_00069]](https://memoriesproject.files.wordpress.com/2014/02/reluctant-caregiver-cover.jpg)