It was a busy year in Alzheimer’s research. In December 2025, the 2025 Clinical Trials on Alzheimer’s Disease Conference was held. The Alzheimer’s Prevention Registry shared highlights from the conference.
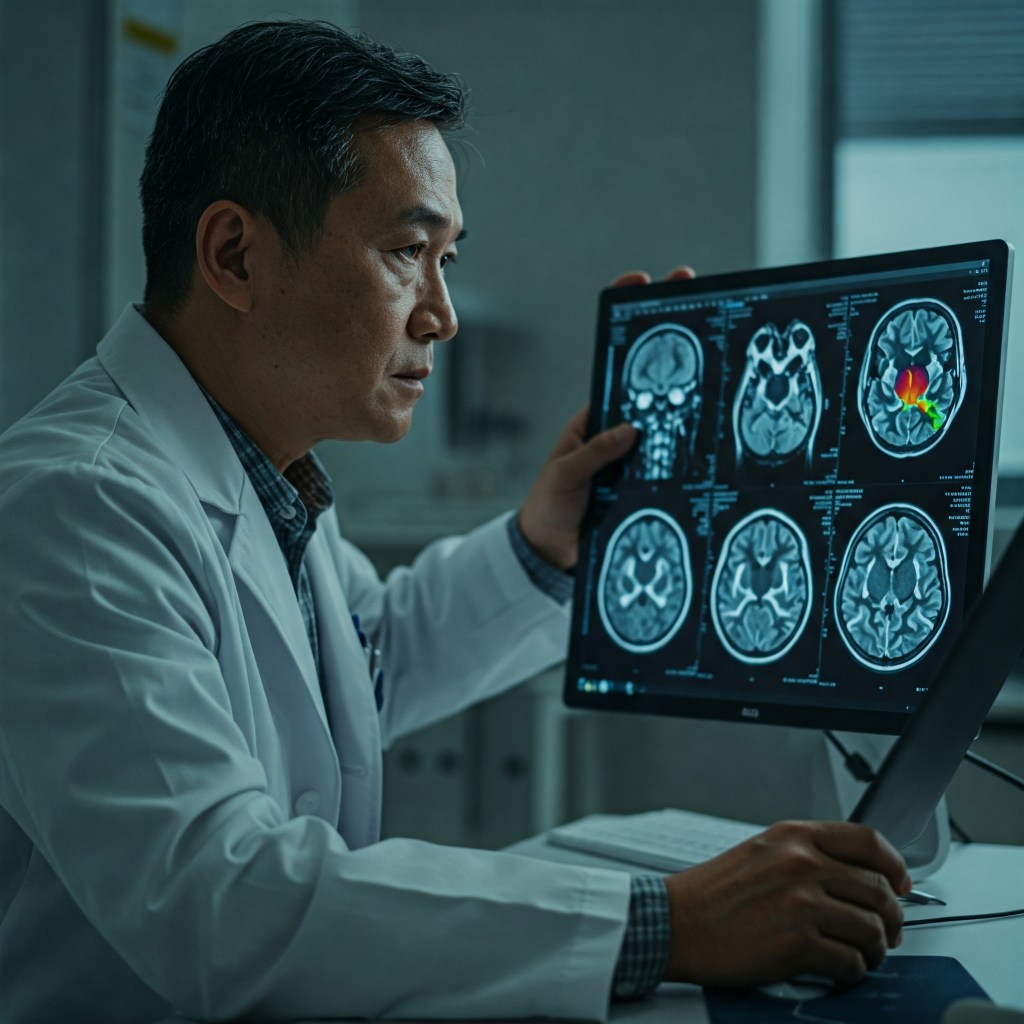
- Blood biomarker testing is an area of research I’ve been closely following. There have been advancements in using blood biomarkers to accurately detect abnormal blood proteins like amyloid and tau. Developing reliable, simpler, and most cost-effective diagnostic methods for Alzheimer’s and other dementias will allow people to be diagnosed and treated sooner, when the currently available treatments are more effective.
- GLP-1s: You may have seen reports about drugs like Ozempic and Mounjaro, which have become popular weight management treatments, may also help reduce brain inflammation and offer other brain protective benefits. Research is underway to see if such drugs could be used to treat or prevent Alzheimer’s and other forms of dementia. Early results were disappointing, as the drugs failed to slow disease progression in people with early-stage Alzheimer’s, but further research will be conducted.
- Lifestyle interventions offer cognitive benefits: I wrote last year about the U.S. Pointer trial findings and how structured lifestyle interventions including diet, exercise, and cognitive training led to improved cognition. At the December conference, more results were shared, including small benefits for those with sleep apnea, which has been linked to an increased dementia risk. Also shared at the conference was research on the benefits of receiving the shingles and TB vaccines.
- Updates on current Alzheimer’s treatments: While there have been controversies about lecanemab and donanemab, the latest research shows that they do help slow the progression of the disease, even after treatment is stopped. This is an important finding as these treatments raise the risk of serious side effects such as brain bleeds. The next generation of anti-amyloid treatments are being developed and tested, with a focus on reducing side effects while offering meaningful benefits.
These findings demonstrate the hard work being conducted by Alzheimer’s researchers to improve testing and develop more effective treatments with fewer side effects. The cognitive benefits of lifestyle changes should not be overlooked, as research continues to find positive impacts in this area.
Image generated by Google Gemini.







![Pageflex Persona [document: PRS0000038_00069]](https://memoriesproject.files.wordpress.com/2014/02/reluctant-caregiver-cover.jpg)