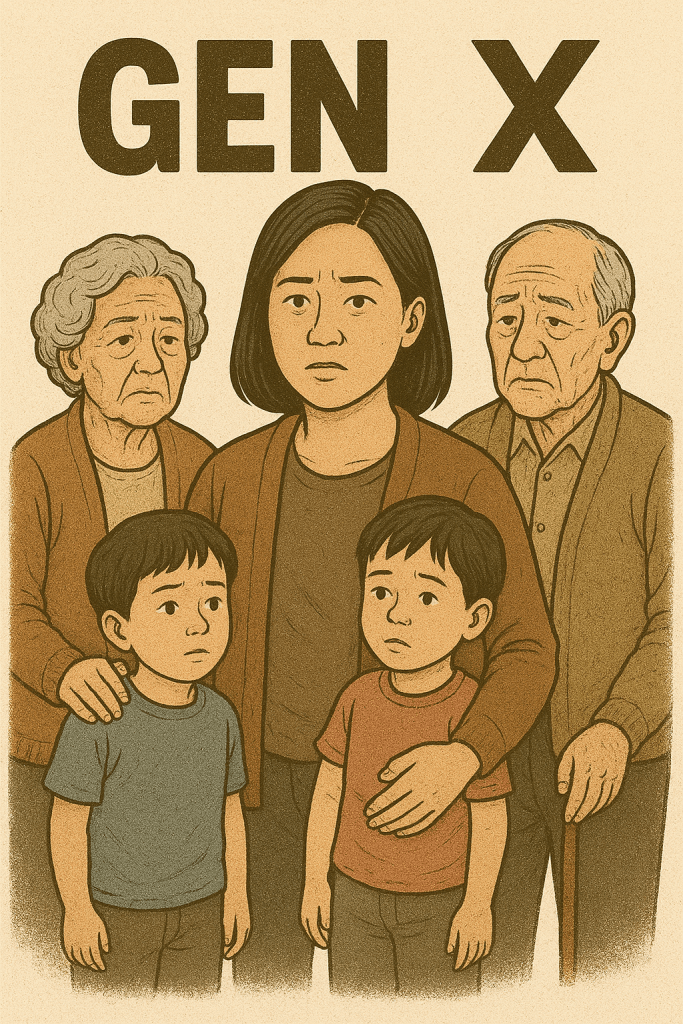
Next Sunday, many Americans will watch the Super Bowl to see who will be crowned this NFL season’s champion. I will be watching and thinking of my father, who learned to love American football though soccer and baseball were dear to his heart as well.
There is a dark side to every sport, and in the NFL, the head trauma risk from the hard-hitting game along with diagnostic and research developments have identified an alarming number of chronic traumatic encephalopathy (CTE) cases among former players. CTE can cause cognitive symptoms that mirror Alzheimer’s and other forms of dementia, such as memory loss, personality changes, mood swings, paranoia, and depression. CTE has been found in the brains of high-profile former NFL players who died of suicide, such as Junior Seau.
In a new study published in January 2026, researchers at the Boston University CTE Center studied over 600 donated brains, mostly of contact sport athletes exposed to repetitive head impacts and found those with the most advanced form of CTE had a four times increased odds for having dementia. The study noted that the increased risk amount is “similar to the strength of the relationship between dementia and advanced Alzheimer’s disease pathology, which is the leading cause of dementia.”
In 2023, the Boston University CTE Center found CTE in 345 of the 376 brains of former NFL players that were donated to its brain bank. Researchers cautioned that donated samples are subject to selection biases and because CTE can only be definitively diagnosed after death, it’s impossible at this time to calculate the current prevalence of CTE among NFL players.
The Boston University CTE Center stresses that the most severe symptoms and outcomes are in the minority of cases they see, and that CTE symptoms are treatable. Former players or anyone who has suffered significant and repeated head trauma should seek professional medical care as soon as symptoms emerge.
I’m grateful to the former NFL players and their families for making the generous decision of brain donation to further the research efforts into CTE. Learnings from CTE research could benefit the spectrum of cognitive-based conditions and spur better, more effective treatment options.
Image generated by Google Gemini.








![Pageflex Persona [document: PRS0000038_00069]](https://memoriesproject.files.wordpress.com/2014/02/reluctant-caregiver-cover.jpg)